Bulk-billed DEXA Scan if eligible upon conditions of Medicare, or else flat fees apply.
*Where Medicare is applicable
Prevention and Diagnosis
– Proactive approach to maintaining bone health and minimizing the devastating effects of osteoporosis
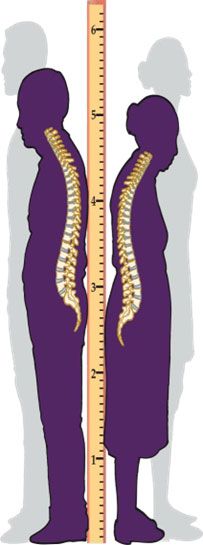
Like other organs in the body, bones are constantly changing. Throughout childhood and young adulthood, bones grow in strength and in size. Around the age of 30, bones reach their peak strength and then naturally become weaker with age. Osteoporosis is a condition where bones become abnormally weak to the point of breaking. This weakening may be caused by other factors that are associated with age. Symptoms of osteoporosis do not occur until a lot of bone strength is already lost. The most visible symptoms may include loss of height, along with curvature of the upper back. Osteoporosis also can result in a crippling and painful fractures, occurring most often in the hip, back, or wrist. Some people are more likely to develop osteoporosis than others. The following risk factors have been identified so that people can be aware if they have an elevated risk. Osteoporosis is especially prevalent among women, who can lose up to 20 percent of their bone mass in the five to seven years after menopause.
“Test Your Bone strength with BMD, not lifting weights”

While there is no cure for osteoporosis, it is treatable. There are many easy steps you can take to manage the disease and reduce your chance of breaking a bone.
It is important to work with your health care provider to assess your risk for osteoporosis and broken bones and to organise a routine follow up regime. Your provider will help access your Medicare eligibility for the test.
Osteoporosis is a condition where bones become thin, weak and fragile. As we age it increases the risk of fracture
DEXA can’t predict but can prevent future bone fractures
People lose height as they age, often because of fractures in their spine. If you are shorter (especially if more than 1-1/2 inches shorter) now than you were in your 20s, you need to be tested
What is osteoporosis?
Osteoporosis literally means “porous bone.” As we age, our bones naturally lose thickness and strength. Osteoporosis leads to an increased risk of fracture. Called the “silent crippler,” it often progresses without symptoms or pain until a fracture occurs. Approximately two out of three women, and one out of three men, as they get older are affected. Hip fractures often result in a loss of independence and the need for nursing home care. The best way to avoid osteoporosis is to determine your risk early and then take steps to prevent the disease. It’s important to start prevention early. Peak bone mass is attained by age 25–30 in women. With proper diet, including calcium, and exercise, you may be able to slow or prevent the onset of osteoporosis. If you already have the disease, early detection and proper medical care can help you slow or even reverse its progress. BMD test can determine the severity of the disease.
Who should have BMD?
Bone loss in women begins at about age 30 and accelerates after menopause. Women over age 50 have the greatest risk for developing osteoporosis, but the disease can strike at any age. It is important to remember that this disease does not only strike women: one in eight men over the age of 50 are at risk of developing osteoporosis.
Risk factors include:
❖ advanced age, female
❖ a history of bone fracture
❖ a small thin frame
❖ a family history of osteoporosis
❖ removal of the ovaries
❖ early menopause
❖ Age (All women over age 65 should have a bone density test
regardless of the presence of any risk factors.)
❖ Absence of menstrual periods (amenorrhea)
❖ Anorexia nervosa or bulimia
❖ Diet low in calcium
❖ Use of certain medications, such as corticosteroids and
anticonvulsants
❖ Low testosterone levels in men
❖ Inactive lifestyle •Cigarette smoking
❖ Excessive alcohol use
❖ Being Caucasian or Asian, although African Americans and
Hispanic Americans are at-risk as well
❖ Diseases such as intestinal problems, kidney problems,
hormonal problems, kidney stones, liver disease
❖ alcohol and tobacco use
❖ vitamin D deficiency
❖ Organ transplant recipients, Crohn’s disease, celiac disease,
Paget’s disease, rheumatoid arthritis
What can I expect during my bone densitometry test?

A certified DXA technologist will perform Dual energy x ray DEXA, which measures bone density, a measure of bone strength. DXA scanners use very low dose X-rays and are considered the Gold Standard for the diagnosis of osteoporosis. A low DXA value is useful in indicating the future risk of breaking a bone. DXA scans are valuable determining the strength of your bones and in monitoring treatment. Osteoporosis can also be provisionally diagnosed if a middle aged or elderly person develops a broken bone (fracture) after minimal trauma. Once a person suffers one such fracture, they are at much higher risk of suffering further fractures.
The bone densitometer is like a large examination table. It is padded and comfortable. Your name, age, height, weight, and ethnicity will be entered into the computer before your test. This information is used to compare your results to a normal reference group. You will be asked to lie on your back, remaining in your normal clothing in most cases. Belt buckles, metal or thick plastic buttons and metal jewellery will need to be removed from the region being examined. The operator will position your arms and legs for the test, which is painless and typically takes 10-15 minutes. You just need to lie still and breathe normally.
A weak beam of x-rays will scan your spine, hip or forearm depending on which scans your doctor has requested. The latest generation of DXA bone scanners can often detect unsuspected spine fractures using a special lateral (side) view of the spine (Lateral Vertebral Assessment). Your doctor may suggest follow-up tests to detect change over time. Don’t panic! – no blood or bone samples are taken, and you are not enclosed in a tunnel.
Is there any preparation?
No preparation required. If possible, please remove any body piercing (e.g., navel rings) or magnets from your torso before the test. Also avoid wearing tight briefs as these may distort the scan image. If you have had a barium, CT scan, radioisotope, or have been injected with any contrast dye (used for testing purpose) you need to wait 14 days before your bone density procedure. Do not take calcium supplements for at least 24 hours before the exam
Is the test safe?
Even though X-rays are used, the amount absorbed by the patient is only about 1/10th of that received from a chest X-ray. The X-ray dose from the bone densitometry test is comparable to the naturally occurring radiation you are exposed to in one week.
Caution: Even though the X-ray dose from the bone densitometry test is very low, please inform the operator if you are pregnant or might be pregnant before your test!
What happens to your results?
Your results will be compared with what is normal for your age and sex and assessed in relation to your future risk of fracture. Your report should reach your doctor in approximately 5-7 working days of your test. Please return to your doctor to discuss the results
Do you need a referral from your doctor?
We cannot scan you without a written request from your doctor. Please make sure you bring your referral with you to your appointment.
Have you had a previous bone density?
Unless your doctor has specified otherwise, you should have your bone density tests at the same practice where you had your original scans. Comparisons between bone density scans obtained at different facilities are not possible as each bone density machine gives a slightly different reading.
*DEXA cannot predict but prevent osteoporosis.
Which lifestyle factors are important?
Regular exercise, adequate calcium in our diets and avoiding smoking or excess alcohol and caffeine, will decrease the risk of osteoporosis. Measures which lower the risk of falling are also important in preventing osteoporotic fractures.
– Reduce fracture risk
– Prevent future broken bone
– Track and increase or decrease of bone mass
– Our focus is your good health
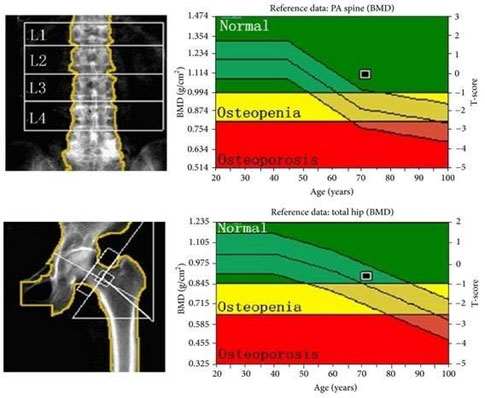
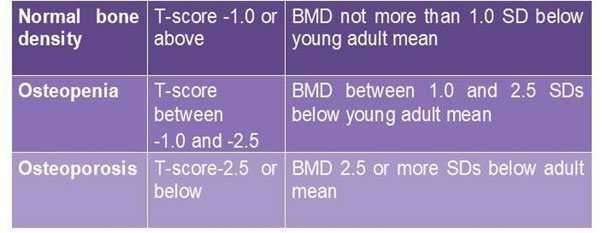
Z-score
The Z-score compares the patient’s bone density to that of adults of the same age. It is the number of standard deviations (SDs) of the BMD measurement above or below that of adults of the same age and sex. Z-score is a useful indicator of possible secondary osteoporosis. A Z-score of -2.0 or below should trigger investigations for underlying disease to exclude other causes of bone mineral loss.
T-score
The T-score compares the patient’s bone density to the peak bone density of young adults. It is the number of standard deviations (SDs) of the BMD measurement above or below that of young healthy adults of the same sex. According to definitions agreed by the World Health Organization, a T-score of -2.5 or lower at the spine or hip is indicative of osteoporosis.
Please contact us if you need to reschedule your appointment
This information is of general nature only and is not intended as a substitute for medical advice. If you have any questions or concerns, please ask your doctor or medical imaging staff. They will be happy to explain.
Cost Information
If eligible and conditions met, we offer bulk-billed bone mineral density scan, in case not eligible, flat fees apply, kindly speak to our admin team for further billing information.
THE NEXT STEP
Please ensure that you have your Medicare card and referral with you and pop into our radiology clinic for your X-ray. If you have any questions at all please feel free to contact us, as we are here to help.

 Serving patients and Saving their lives
Serving patients and Saving their lives